Red Flag Tumour 3
Here is the third in this series of Red Flags - Tumor articles. The previous ones can be accessed via links;
Clinical History 21 yo female, no children
June
Fulltime hairdresser, playing netball and attending aerobic classes for fitness. She developed L-sided rib pain that was limiting her from sleeping as the pain prevented her from lying on that side while trying to sleep. No other sport or ADLs could be completed during the diagnosis period.
She was living in Perth at the time and visited a GP, who palpated left rib 5 and said, ‘feels like cysts, not right, need to get sorted’. Arranged for an US but not undertaken as was moving to Esperance.
July
In Esperance, she went to a new GP and had US (23/7 reported as normal).
October
Pain persisted. Seen by another GP in the same clinic and told nothing was wrong, but the client pushed for more intervention. With reluctance, GP was referred for XR 14/11, which was reported as normal.
December
She returned to the same clinic and was seen by a locum GP. GP listened and explained not happy with the symptoms and referred them to Kalgoorlie for CTS.
CTS Result. 3cm craniocaudal * 3cm transverse * 7.5cm antroposterior tumor with several 2-3cm haemorrhagic fluid cysts and partial erosion of 5 ribs.
The client was happy that something had been found (as previous visits to GP stated nothing was wrong and intimated she was catastrophising) and spent the day in Kalgoorlie shopping.
Returned to Esperance, and reality set in. Immediately went to Perth for blood tests, MRI and CT needle biopsy and specialist consultation.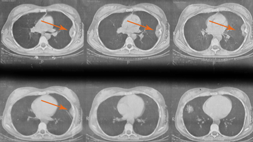
Surgery was planned, but the surgeon carried out an open biopsy instead. Then, she had four sessions of chemotherapy over 3 weeks, which reduced tumour size by 70%.
Surgical excision was carried out on portions of the 5th rib (1 inch around the tumour site) and replacement with mesh membrane. A further 12 chemotherapy sessions were performed as follow-up.
CTS of Thoracic Spine
- Original Scans - see picture (orange arrows)
- Subsequently, had annual CTS for 5 years
- Now has annual XR
Osteosarcoma
Osteosarcoma is a malignant bone tumour that usually develops during rapid growth in adolescence, as a teenager matures into an adult.
Incidence
Osteosarcoma is the eighth most common form of childhood cancer, comprising 2.4% of all malignancies in pediatric patients and approximately 20% of all primary bone cancers. Osteosarcoma is also commonly seen in people over age 60.
Incidence rates in U.S. patients under 20 years of age are 5.0 per million per year and slightly more common in males than females.
This cancer occurs most commonly in larger bones (metaphyseal region) and in the area of bone with the fastest growth rate. However, osteosarcoma can occur in any bone, with 42% femur, 19% tibia, 10% humerus, 8% skull and jaw, and another 8% in the pelvis. No mention of presentation in ribs.
Risk Factors & Cause
Currently unknown cause. In some cases, osteosarcoma runs in families with at least one gene linked to increased risk. This gene may be associated with familial retinoblastoma, an eye cancer.
Management
Treatment starts with a biopsy to confirm the diagnosis, chemotherapy to reduce the size of the tumour and reduce the likelihood of metastasis, followed by surgery to remove the tumour and affected tissue. Long bone tumours may occasionally require limb removal.
What did I Learn?
While I have seen other osteosarcomas, I present this case study because it is a good example of keeping an open mind. This client wasn’t in an active growth pattern at 21 nor over 60, and the site of the presentation was so uncommon it isn’t even listed.
While not a client of mine during the presentation, she could have easily presented with similar symptoms for treatment. I ask myself, would I have picked it up?
Subjectively, the key factors that I would have been considering from the history were;
- non-trauma presentation
- the unremitting pain
- not mechanically aggravated
- easily localised to a specific tissue
- client knowing something ‘was not right’ in her body
Objectively, ADLS and presumably active movements were normal, but palpation revealed to her first GP changes in bony edges. I believe a physiotherapist with sound palpation skills and an inquisitive disposition would have detected similar findings without a history of trauma (past or recent) considered important.
Regarding prior imaging, US distinguishes between solid and cystic masses. The main limitation of XR in imaging malignant bone involvement is that considerable bone destruction must be present before bone metastasis is evident radiographically. It has been estimated that 30–75% reduction in bone density is required to visualize a metastasis on XR. Therefore, the detection of metastasis may be delayed by several months, as was the case in this situation.
Recent Blogs of Interest
- Frustrated with Home Exercise Program Compliance? - VideoXs Solution
- 2013 Confirmed Courses including the New Courses
- Updated Free Resources section including text books, Screening Tools and Outcome Measures
All the best,
Dr Doug Cary PhD
Specialist Musculoskeletal Physiotherapist
AAP Education Clinical Director
Receive a FREE Information Report
Examples include;
- Resource 1. Calcific Tendinopathy: A personal and professional perspective
- Resource 2. Fibromyalgia Syndrome
- Resource 3. Needling and Infection Control Guide v3.2
- Resource 4. Sleep Hygiene Guide - 16 Key Tips
- Resource 5. Step-by-Step Guide to Managing Acute Back Pain
- Resource 6. The Top 7 App Guide

